Endometriosis, what is it?
In order to understand this properly, it is important for you to know about the structure of your body, its hormonal control and your monthly menstrual cycle.
Endometriosis – what is it?
In order to understand this properly, it is important for you to know about the structure of your body, its hormonal control and your monthly menstrual cycle.
For this reason, these topics are presented first.
However, this website is no substitute for a detailed consultation with your doctor. It should be an opportunity for you to inform yourself in peace and quiet at home – also with your partner – so that you can address the individual questions that arise during your next visit to the doctor.
If you are unclear about some of the terms used on this website or that you have heard in connection with the clinical picture of endometriosis, please take a look at our small lexicon “Terms relating to endometriosis”.
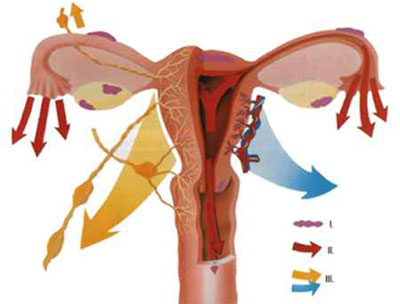
The monthly cycle is controlled by a system that includes the hypothalamus, the pituitary gland and the ovaries.
The central control system in the brain (hypothalamus) influences the appendage gland, which in turn stimulates the ovaries via other hormones. As a result, one egg normally matures per cycle and is released during ovulation so that it can be fertilized by sperm.
The hormones of the ovary (oestrogens and progestrone) lead to the build-up of the uterine lining (endometrium). They are first formed by the follicle and then, after ovulation, by the corpus luteum.
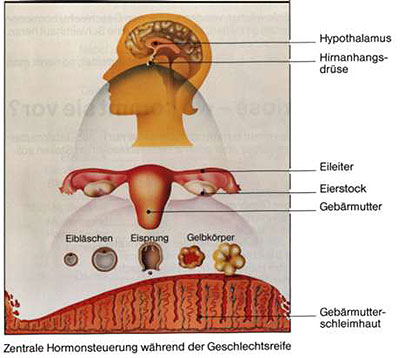
A mucous membrane grows in the uterine cavity every 4 weeks, controlled by the female sex hormones (oestrogen, progesterone). It is used for the implantation of a fertilized egg.
If such a mucous membrane also grows outside the uterus, it is called endometriosis.
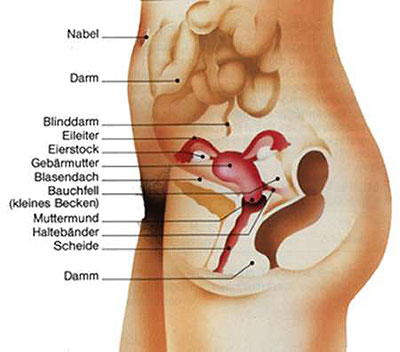
The lining of the uterus normally only occurs in the uterine cavity. However, it can also occur in different parts of the body.
A distinction is made:
- Endometriosis in the genital area, etc.
in the uterine wall in the fallopian tube
in the ovary - on the ligaments holding the uterus
- on the peritoneum of the small pelvis
- on the urinary bladder (e.g. bladder roof)
- in the sheath
- Endometriosis outside the genital area, including the bowel and navel
In rare cases, the lungs, liver, skin and other organs may be affected.
All girls and women who have menstrual bleeding.
Endometriosis tissue is similar to that of the uterine lining. Its growth is mostly hormonally controlled. This is why endometriosis lesions can bleed like the uterine lining. The only difference is that the shed tissue does not leave the body through the vagina, but remains in the body. It accumulates in the abdominal cavity behind the uterus, for example, from where it is slowly reabsorbed by the body. If the blood accumulates, e.g. in a focus of endometriosis in the ovary, endometriosis cysts form. These are also called chocolate or tar cysts because of their bloody brown contents.
First of all, the menstrual cycle, which takes place once a month during sexual maturity, should be explained.
The monthly cycle
Most women have a 28-day (+/- 2 days) menstrual cycle. A cycle with ovulation and normal production of oestrogen and progesterone is a prerequisite for pregnancy.
A cycle begins on the day of menstruation (duration approx. 4-6 days). It is caused by rejection of the uterine lining if pregnancy has not occurred.
Cycle without fertilization
In a normal cycle, ovulation occurs around day 14.
If the egg remains unfertilized, i.e. if a fertilized egg fails to implant in the uterine lining, the corpus luteum regresses and oestrogen and progesterone levels fall sharply by the 28th day. This initiates the shedding of the mucous membrane; menstrual bleeding begins.
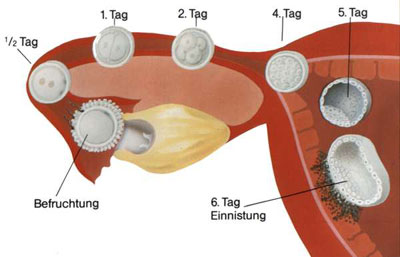
Cycle with fertilization
If an egg is fertilized, it normally implants in the uterine cavity after 6-7 days and releases hormones to the mother (human chorionic gonadotropin, abbreviated to HCG). This stimulates the corpus luteum and causes an increase in oestrogen and progesterone. This prevents the endometrium from shedding; the period “falls out”.
After ovulation, the egg enters the fallopian tube where it is fertilized. Within 5-6 days, the fertilized egg migrates through the fallopian tube into the uterine cavity. It nests there and develops over 9 months into a child ready for birth.
The general incidence in women is reported in the literature to vary between 2 and 10%. In women who are infertile, endometriosis is detectable in over 50% of cases.
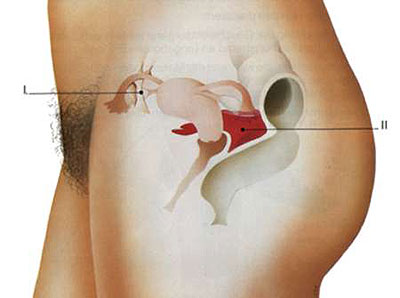
One of the causes of infertility is that due to endometriosis in the small pelvis
I. adhesions, e.g. between the fallopian tube and the ovary, which hinder ovulation and the egg collection mechanism, and
II. biochemical processes take place that can prevent the egg and sperm cell from uniting.
It is not yet possible to make a definitive statement on this question.
The following theories are discussed:
I. During the development of the reproductive organs, “scattered endometrial cells” settle in a different location (congenital endometriosis).
II. Endometrial cells, which are normally shed into the vagina during menstruation, “migrate” through the fallopian tubes into the pelvis and grow there.
III. Endometrial cells are transported via the lymph and bloodstream to distant organs, e.g. lungs.
Endometriosis can cause various symptoms.
There are endometriosis patients who are completely symptom-free. Others have severe pain, behind which other causes are often suspected. The symptoms also depend on the location of the foci and are usually related to menstruation.
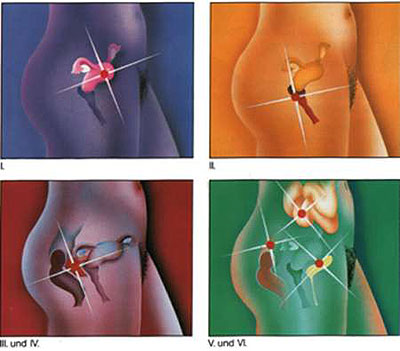
Endometriosis can occur
- in the uterine muscles
=> Pain in the uterus shortly before or at the start of menstruation - in the vaginal area
=> Pain during sexual intercourse or gynecological examinations - in the peritoneum in the small pelvis
=> Frequent infertility, unclear general complaints - in the ovary
=> Ovarian pain, cysts, infertility - in the intestinal wall
=> Intestinal bleeding, intestinal pain, appendicitis pain, etc. - in the bladder wall
=> Irritable bladder, blood in the urine
Your symptoms or the problem of infertility make your doctor think of endometriosis.
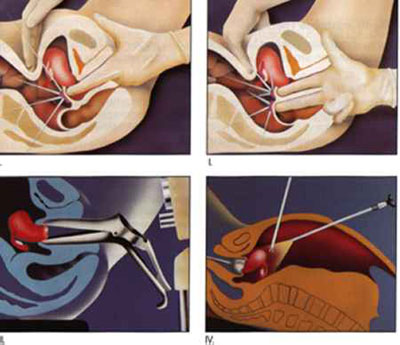
It is recognized by
- gynecological examination
Palpation of the genital organs through the vagina, rectum and abdominal wall - Colposcopy
The cervix and posterior vaginal vault are inspected with the aid of an optical device under 5-10x magnification. - Ultrasound examination
Ultrasound is used to detect ovarian changes, endometriosis lesions or a pool of blood behind the uterus, etc. - laparoscopy
The doctor looks into the abdominal cavity with an endoscope and may take small tissue samples for microscopic examination - Other examinations and interventions
Cystoscopy, colonoscopy, during operations
- Drug therapy
The doctor prescribes medication for this purpose.
They change the hormone production in their body in order to achieve a regression of the endometriosis. 70% of endometriosis lesions are subject to hormonal influence. The reaction to the hormones is primarily controlled by hormone receptors in the tissue. The success of drug therapy therefore depends on whether the endometriosis lesions have hormone receptors or not. However, drug treatment also suppresses the growth of the uterine lining, which means that menstruation usually stops. At the same time, the growth of endometriosis lesions is inhibited and their regression is induced. Your doctor will select the most suitable medication for you. It is important that you take this regularly in the prescribed dosage. This is the only way to achieve an effective inhibitory effect on endometriosis; please note that there may be side effects when taking medication. Your doctor will discuss this with you. - Surgical therapy
The aim of surgical treatment is to suppress endometriosis by removing the endometriosis tissue as completely as possible. Depending on the extent and localization, this is performed by laparoscopy, abdominal incision or surgery from the vagina. - Combination therapy
In some cases – particularly in patients with pain and advanced stages – it may be necessary to follow up surgery with drug therapy. This means that even the smallest foci or surgically inaccessible endometriosis deposits can be removed. In special cases, the so-called “three-phase therapy” has proved successful, i.e. in the third phase of the therapy concept – after 6-9 months of hormonal treatment – any remaining residues are removed by a new laparoscopy. For long-term suppression of endometriosis, these surgical and drug therapy combinations are in the foreground, although there is no real prophylaxis as the cause of the disease is still unknown.
This clinical picture must not be considered in isolation from the physical aspect, as psychological conflicts and stress factors must also be taken into account.
Many patients
- have been under psychological pressure for years because they are afraid to talk about their problems and pain.
- consider pain before and during menstruation to be normal and do not mention it during their visit to the doctor
- suffer from childlessness and are not informed about appropriate treatment options
A few words at the end
This website is intended to inform you that it is important to have an early and accurate medical examination for endometriosis.
The aim of endometriosis treatment is, on the one hand, to achieve freedom from symptoms and well-being for you and, on the other hand, to fulfill any existing desire to have children.
